Understanding Keratoconus: Causes, Risks, and Management
Keratoconus is a condition that affects the shape and structure of the cornea, the clear, dome-shaped surface that covers the front of the eye. The cornea’s job is to focus light onto the retina, helping us see clearly. In keratoconus, the normally round cornea becomes thin and bulges out into a cone-like shape, which causes distorted vision. But what exactly causes keratoconus? Let’s explore its causes, risk factors, and how it’s managed.
The exact cause of keratoconus is not fully understood, but both genetic and environmental factors seem to play a role. Around 8% of cases may be due to genetic mutations, while 92% could be influenced by environmental factors, such as eye rubbing, which is often linked to allergies. While keratoconus can run in families, it’s not a predictable or obvious genetic inheritance pattern. If someone in your family has keratoconus, you might have a higher chance of developing it, but this isn’t guaranteed.
Keratoconus is often associated with certain medical conditions. People with Down syndrome, Leber’s congenital amaurosis, and Ehlers-Danlos syndrome (a connective tissue disorder) tend to develop keratoconus more often than those without these conditions. Eye rubbing is also a significant factor. When individuals with a genetic predisposition rub their eyes frequently—often because of conditions like allergies or eczema—it may contribute to keratoconus developing or worsening.


Key Risk Factors
Keratoconus doesn’t have one single cause, but certain factors can make it more likely:
- Eye rubbing: This is one of the strongest links. People with allergies or conditions like vernal keratoconjunctivitis (a type of eye inflammation) are more likely to rub their eyes, increasing their risk.
- Sleep apnoea: There’s a higher occurrence of keratoconus among people with sleep apnoea.
- Connective tissue disorders: Conditions like Ehlers-Danlos syndrome or Marfan syndrome are linked to keratoconus.
- Floppy eyelid syndrome: A condition where the upper eyelids are unusually loose and rubbery, making them prone to folding backward.
- Retinitis pigmentosa: A group of inherited disorders that affect the retina and cause vision loss.
- Positive family history: If keratoconus runs in the family, your chances of getting it are higher.
- Down syndrome: People with Down syndrome have a higher likelihood of developing keratoconus.
- Pregnancy and hormonal changes: Some evidence suggests that the hormonal shifts during pregnancy can lead to or worsen keratoconus.

How Keratoconus Affects the Eye
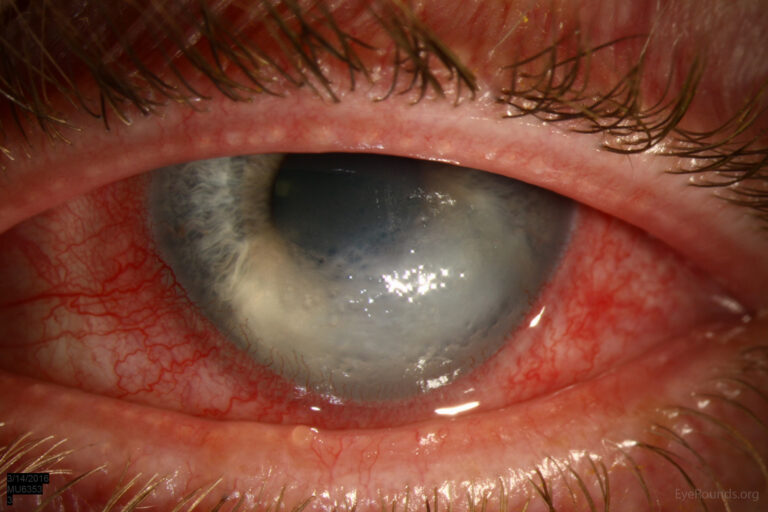
Keratoconus leads to distinct structural changes in the cornea. Pathologists have observed thinning of the corneal layers, fragmentation in Bowman’s layer (a thin protective layer in the cornea), and scarring. The cornea also loses its regular shape and becomes cone-shaped, causing vision problems. This happens because the proteins in the cornea, which normally hold it in place, start to weaken. Some research suggests that enzymes and other molecules like cytokines and free radicals contribute to the breakdown of the corneal structure, adding an inflammatory component to the disease.
Preventing Keratoconus
Unfortunately, there are no foolproof ways to prevent keratoconus. However, there are some steps you can take to minimize the risk:
- Avoid rubbing your eyes: Since eye rubbing is a known factor in the progression of keratoconus, keeping your hands away from your eyes can be helpful. If you have allergies that make your eyes itchy, consider using allergy eye drops or antihistamines to reduce irritation.
- Manage allergies: Treating conditions that make you rub your eyes—such as hay fever, eczema, or conjunctivitis—can help.
- Screening children in school: Early detection is key to slowing down the progression of keratoconus.
- Avoid rubbing your eyes: Since eye rubbing is a known factor in the progression of keratoconus, keeping your hands away from your eyes can be helpful. If you have allergies that make your eyes itchy, consider using allergy eye drops or antihistamines to reduce irritation.
- Manage allergies: Treating conditions that make you rub your eyes—such as hay fever, eczema, or conjunctivitis—can help.
- Screening children in school: Early detection is key to slowing down the progression of keratoconus.
Diagnosing Keratoconus
Keratoconus is often diagnosed during a routine eye exam. Eye doctors use special tools to check for the early signs of the condition. A slit-lamp examination is one method used to detect thinning or bulging in the cornea. Another technique, called computerized videokeratography, creates a detailed map of the cornea, which can show even the smallest changes in its shape.
Keratoconus often starts in both eyes, but it usually affects one eye more than the other. Symptoms can appear as early as adolescence and tend to worsen through the twenties and thirties, though this isn’t always the case. In some individuals, keratoconus can remain mild throughout life. Signs to watch for include frequent changes in prescription glasses or a sudden inability to see clearly with your usual glasses. Many people with keratoconus initially use soft contact lenses, but as the condition progresses, they may need specialized contact lenses, such as rigid gas-permeable (RGP) lenses, which can better correct vision.
What Are the Symptoms?
Keratoconus symptoms often start with mild blurring of vision and may worsen over time. Here’s what to look for:
- Distorted vision: Objects may appear stretched or blurry.
- Frequent prescription changes: If you’re needing to update your glasses or contact lenses often, this could be a sign of keratoconus.
- Light sensitivity: Bright lights may cause discomfort or halos.
- Difficulty seeing clearly with glasses: Many people find that glasses don’t fully correct their vision, and contact lenses provide better clarity.
Diagnostic Tests
- Slit-lamp exam: This checks for signs of corneal thinning.
- Retinoscopy: A test that looks for a “scissoring” reflex, which indicates irregular astigmatism.
- Keratometry or computerized corneal topography: These measure the curvature of the cornea.
- Pachymetry: An ultrasound test that measures the thickness of the cornea.
- Tear film biomarkers: Some researchers are exploring whether certain markers in the tears of keratoconus patients could help in diagnosis.
Managing Keratoconus: Treatment Options
The treatment for keratoconus depends on the severity of the condition. For mild cases, glasses or soft toric contact lenses might be enough to correct vision. As the condition progresses, RGP contact lenses are often required. These lenses offer more rigid support to help the cornea maintain its shape.
For more advanced cases, there are several other options:
- 1. Corneal Collagen Cross-Linking (CXL): This is a relatively new treatment that can stop the progression of keratoconus. It works by strengthening the cornea. During the procedure, the doctor applies riboflavin (vitamin B2) to the cornea and activates it with UV light. This helps to create new bonds between collagen fibers in the cornea, making it more rigid. CXL doesn’t reverse the condition, but it can prevent further thinning and distortion.
- Specialty Contact Lenses: If glasses and regular contact lenses don’t work, there are other options like scleral lenses, which are larger and sit on the white part of the eye (sclera) rather than directly on the cornea. This can provide more comfort and better vision for people with keratoconus.
- Surgical Options: In cases where the cornea is severely scarred or damaged, surgery may be necessary.
- Intrastromal Corneal Ring Segments (ICRS): These are small rings implanted in the cornea to help flatten its shape. This can reduce some of the irregularities and make wearing contact lenses easier.
- Corneal Transplant the most severe cases, a corneal transplant (keratoplasty) may be required. In this procedure, the damaged cornea is replaced with healthy donor tissue. While this is generally successful, it comes with risks like rejection of the donor tissue and the need for long-term medication.
- Management of Acute Hydrops: In rare cases, a sudden complication known as acute corneal hydrops can occur. This happens when the inner layer of the cornea (Descemet’s membrane) breaks, causing swelling and sudden vision loss. In these cases, treatment involves managing the symptoms with saline drops, pressure patches, and sometimes surgery.

Follow-up and Monitoring
Once diagnosed with keratoconus, regular follow-up appointments are crucial. Eye doctors typically monitor changes in the cornea every 3-6 months, especially in younger patients or those with progressing disease. The goal is to catch any worsening early so that treatments like CXL can be applied promptly to preserve vision.
For patients using contact lenses, these follow-ups also provide an opportunity to reassess lens fit and comfort. Proper care of lenses is essential, as poorly fitting lenses can irritate the cornea and worsen the condition.
Surgery and Post-Op Care
If surgery is required, such as corneal transplants or ring segment implants, patients need to be followed closely during the healing process. Vision correction will likely still be necessary after surgery, whether through glasses or contact lenses. Additionally, patients need to be monitored for complications like infection or graft rejection, which can occur after a corneal transplant.
In conclusion, while keratoconus can significantly impact vision, early detection and intervention can preserve eye health and maintain quality of life. From avoiding eye rubbing to exploring advanced treatments like corneal cross-linking, there are many options for managing keratoconus and preventing further vision loss. Regular eye check-ups and following the advice. of your eye care team is very important.