No more corneal transplants – EVER!
A recent patient was a 18-year-old boy with advanced keratoconus – He came to us as he failed his vision test for a driving licence. The surprise was that his father’s sight was also severely limited due to very advanced keratoconus. His father had needed corneal transplants in both eyes. My plan is to break this cycle. I want to ensure that this boys’ children will have their keratoconus treated early so that they will have all the freedoms and advantages that come with having vision good enough to get their driver’s licence.
Without screening our kids are going blind – FACT!
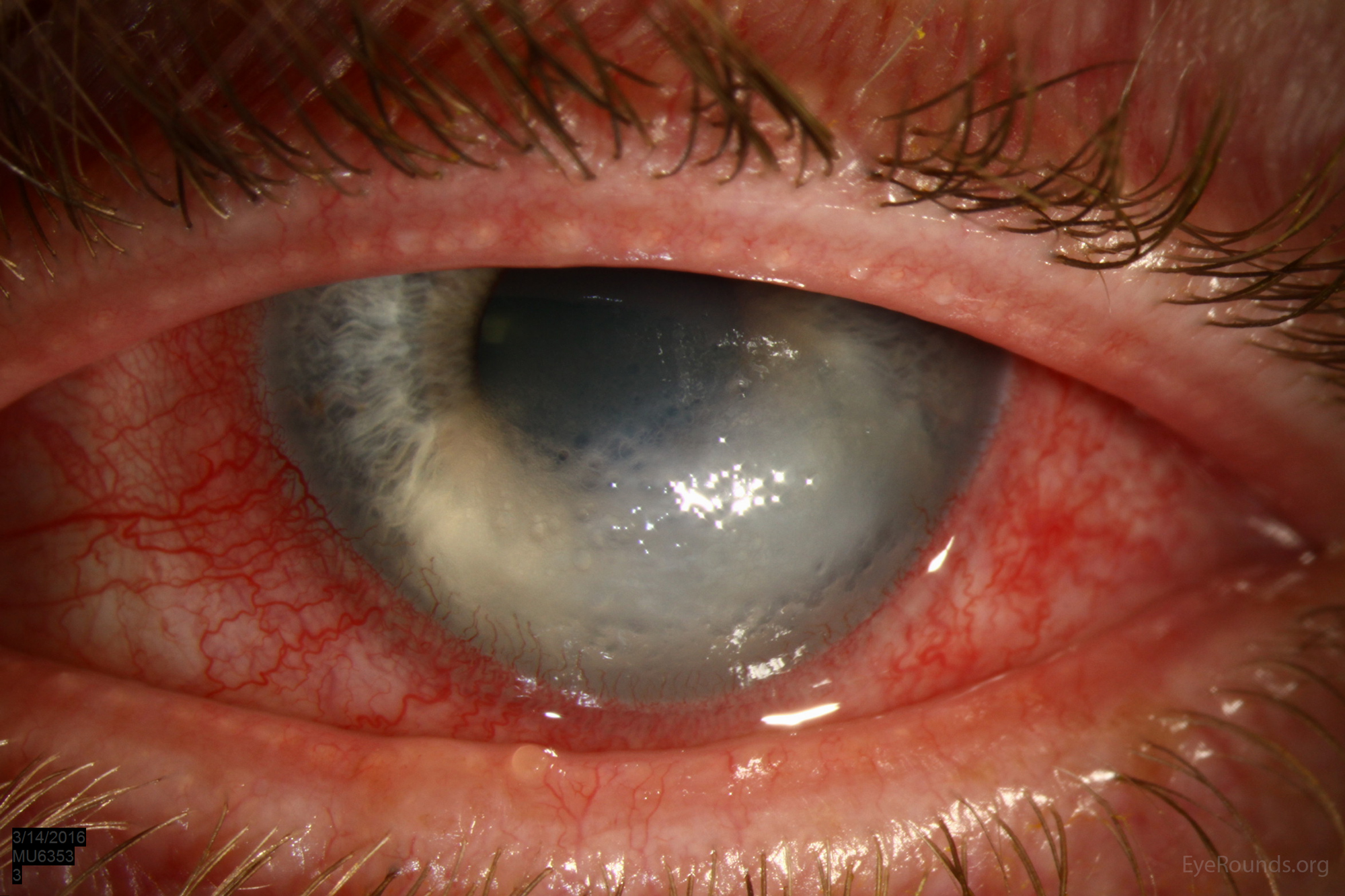
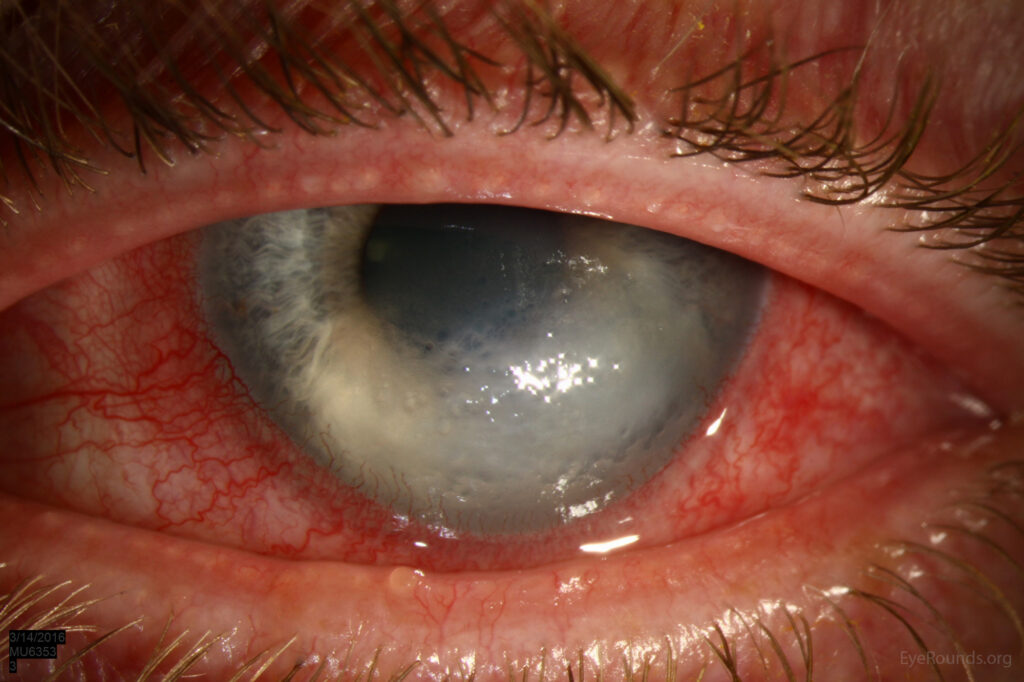
They go blind through a painful process called Acute Hydrops – 18 months of pain then a scar in the front of their eye.
For decades, corneal transplants have been the mainstay treatment for advanced keratoconus—a progressive eye condition that can blind people. But what if we told you that the need for corneal transplants could one day become a thing of the past? With early screening for keratoconus and prompt intervention, this vision is closer than we think.

Understanding Keratoconus and Its Impact on Vision
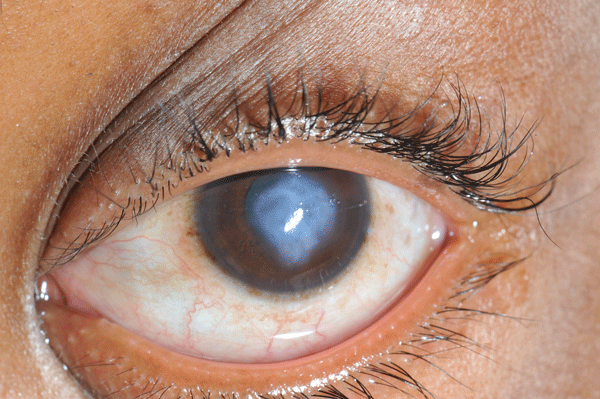
Keratoconus is a condition where the cornea, the clear front surface of the eye, thins and bulges outward in a cone-like shape. This irregular shape distorts light entering the eye, leading to blurred or distorted vision. In its early stages, keratoconus can often be managed with glasses or contact lenses.
However, if it progresses to an advanced stage, the thinning becomes so severe that some people develop a very painful condition called corneal hydrops. This eventually forms a scar; a corneal transplant may be the only option to restore functional vision.
In fact, keratoconus is a leading cause of corneal transplants worldwide, especially in younger individuals.
The disease typically begins in intermediate and high school ages and continues into the 20s, significantly impacting one’s education, career, and quality of life. That’s why early diagnosis and intervention are essential in managing keratoconus effectively.
Why Screening All Children for Keratoconus Could Change Everything
The ability to detect keratoconus early has vastly improved over the years, thanks to advances in corneal imaging technology. Today, withing a few seconds, we can identify signs of keratoconus even in its subclinical stages. This is well before vision is noticeably affected. By implementing routine screenings in children Cone.org.nz will detect the onset of keratoconus in its earliest stages.
Such screenings allow us to:
1. Diagnose the condition early:
Through screening our whānau in school allows early detection, this means we can intervene before the disease progresses. Often before they know that they have the disease.
2. Monitor progression:
After screening with Cone.org.nz affected students will attend the Rotorua Eye Clinic and other centres offering corneal cross-linking treatment. Regular follow-up appointments can help eye doctors understand how rapidly the keratoconus is progressing and determine the optimal time for treatment.
Crosslinking: The Game-Changer in Keratoconus Management
One of the most promising developments in recent years has been corneal collagen crosslinking (CXL). Crosslinking is a 30 minute, minimally invasive procedure that uses ultraviolet (UV) light and riboflavin (vitamin B2) drops to strengthen the collagen fibres in the cornea. This stabilizes the cornea, halting the progression of keratoconus and preserving the patient’s existing vision. It cannot reverse the damage done but can halt further progression.
Crosslinking has revolutionized keratoconus treatment because it can stop the disease in its tracks. When performed at the right time—ideally in the early stages of keratoconus.

Crosslinking can prevent the cornea from deteriorating. Preventing the need for corneal transplants!
The Potential Impact of Nationwide Screening and Early Crosslinking
It is our dream that one day every child will be screened for keratoconus during their time in school. Detecting keratoconus early, combined with crosslinking, will lead to a future where corneal transplants for keratoconus are no longer necessary. Here’s how this proactive approach could help:
Preservation of Vision:
Crosslinking can halt the progression of keratoconus, preserving good vision and preventing the need for more invasive procedures.
Better Quality of Life:
Patients who undergo crosslinking early often experience minimal disruption to their daily lives, as they avoid the lengthy recovery process and potential complications associated with corneal transplants. Currently the waiting time for a person to have a corneal graft is over 1 year. In New Zealand there are not enough donors for all the people who need corneal grafts. For some patients we need to purchase donated corneas from other countries.
Reduced Healthcare Costs:
Corneal transplants are not only costly but also require long-term follow-up, medication, and often additional surgeries. By replacing these with a single, minimally invasive procedure, the healthcare system could save considerable resources.
Is It Realistic?
While it may sound ambitious, this vision isn’t as far off as one might think. Here at Cone.org.nz we are starting in November 2024 to screen around 1,000 children at 2 of our local schools. In Term 1 of 2025 we will start to screen around 6,500 children throughout Rotorua. We plant to extend our screening to surrounding areas. We are working with the Ministry of Education to get information on keratoconus as part of the school curriculum. We work with the Ministry of Health through our Eye Health Clinical Networks to establish a national Screening Program for New Zealand.
Conclusion: A World Without Corneal Transplants for Keratoconus?
The need for corneal transplants from keratoconus could be drastically reduced—and perhaps eliminated—if all children were screened for keratoconus and crosslinking was readily available for those diagnosed. This approach would not only preserve vision for millions but also empower individuals to lead lives free from the limitations imposed by this progressive eye disease.
In the future, early detection and crosslinking might just make corneal transplants a rare exception rather than the standard of care for keratoconus. It’s a vision worth striving for, and with the right tools and support, we can make it a reality.